HIV Vaccines
Topics
What Are Vaccines and What Do They Do?
Vaccines are products made from very small amounts of weak or dead germs (such as viruses, bacteria, or toxins) that can cause diseases. They help your immune system fight infections faster and more effectively.
When you get a vaccine, it sparks your immune response, helping your body fight off and remember the germ so it can attack it if the germ ever invades again. And since vaccines are made of very small amounts of weak or dead germs, they won’t make you sick.
Vaccines are usually administered by a shot, but sometimes can be administered by mouth or nasal spray. They are widely used to prevent diseases like polio, chicken pox, measles, mumps, rubella, influenza (flu), hepatitis A and B, and human papillomavirus (HPV).
Learn more about how vaccines protect you and others.
Is There a Vaccine to Prevent HIV?
No. There is currently no vaccine available that will prevent HIV infection or treat those who have it.
However, scientists are working to develop one. NIH is investing in multiple approaches to prevent HIV, including a safe and effective preventive HIV vaccine.
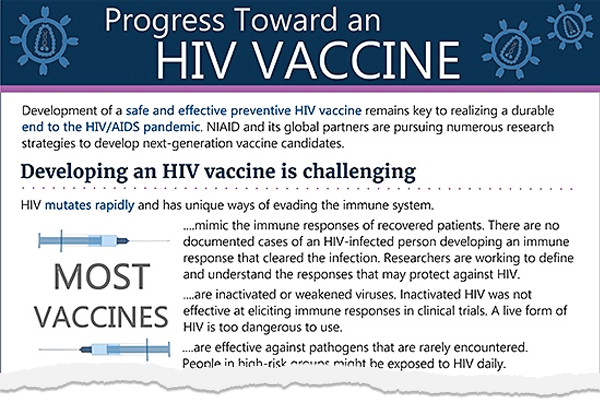
Download NIAID's Progress Toward an HIV Vaccine fact sheet
Other NIH-supported research aims to deliver additional HIV prevention options that are safe, effective, and desirable to diverse populations and scalable worldwide to help end the global pandemic.
Learn more about how the National Institute of Allergy and Infectious Diseases, part of NIH, is approaching HIV vaccine development.
Why Do We Need a Vaccine to Prevent HIV?
Today, more people living with HIV than ever before have access to life-saving treatment with HIV medicines (called antiretroviral therapy or ART), which is good for their health. When people with HIV take HIV medicine as prescribed and get and keep an undetectable viral load, they can live long and healthy lives and will not transmit HIV to their HIV-negative partners through sex. In addition, people who are HIV-negative and who are at risk for HIV infection can take pre-exposure prophylaxis (PrEP), HIV medicine used to prevent HIV. Yet, unfortunately, in 2019, an estimated 34,800 new HIV infections occurred in the United States, and approximately 1.5 million people newly acquired HIV worldwide. To control and ultimately end HIV globally, we need a powerful array of HIV prevention tools that are widely accessible to all who would benefit from them.
Vaccines historically have been the most effective means to prevent and even eradicate infectious diseases. They safely and cost-effectively prevent illness, disability, and death. Like smallpox and polio vaccines, a preventive HIV vaccine could help save millions of lives.
Developing safe, effective, and affordable vaccines that can prevent HIV infection in uninfected people is the NIH’s highest HIV research priority given its game-changing potential for controlling and ultimately ending the HIV/AIDS pandemic.
The long-term goal is to develop a safe and effective vaccine that protects people worldwide from acquiring HIV. However, even if a vaccine only protects some people who get vaccinated, or even if it provides less than total protection by reducing the risk of infection, it could still have a major impact on the rates of transmission and help control the pandemic, particularly for populations at high risk of getting HIV. A partially effective vaccine could decrease the number of people who acquire HIV, further reducing the number of people who can pass the virus on to others. By substantially reducing the number of new infections, we can stop the epidemic.