The Affordable Care Act and HIV/AIDS
Topics
Improving Access to Coverage
The Affordable Care Act (ACA) provides Americans—including those with and at risk for HIV—better access to health care coverage and more health insurance options.
Health insurance gives people with HIV access to appropriate HIV medical care, particularly treatment with HIV medicine called antiretroviral therapy (ART), which helps people with HIV stay healthy and prevent transmitting HIV to others.
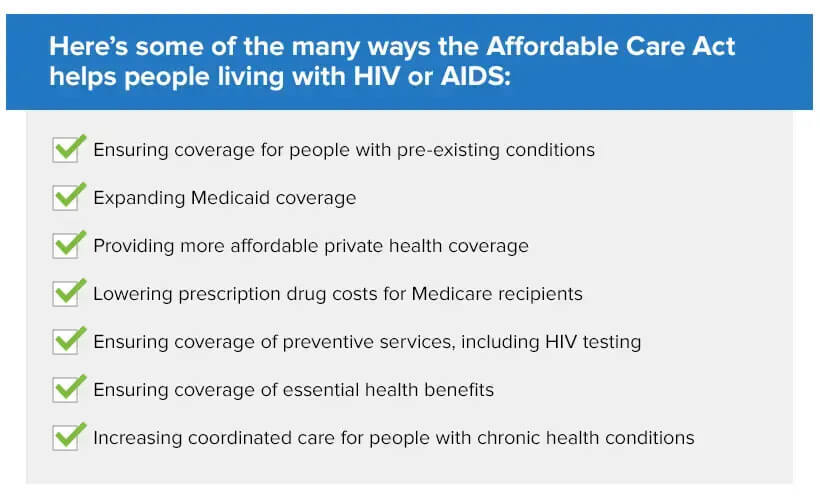
Here are just some of the ways the ACA has improved access to coverage for people with or at risk for HIV:
Coverage for people with pre-existing conditions. Thanks to the ACA, no American can ever again be dropped or denied coverage because of a pre-existing health condition, like asthma, cancer, HIV, or COVID-19. Insurers also are prohibited from cancelling or rescinding coverage because of mistakes made on an application and can no longer impose lifetime caps on insurance benefits. These changes are significant because prior to the ACA, many people with HIV or other chronic health conditions experienced obstacles in getting health coverage, were dropped from coverage, or avoided seeking coverage for fear of being denied. Now they can get covered and get the care they need. (Learn more: The Access, Care, & Engagement TA (ACE TA) CenterExit Disclaimer provides tools and resources to support the enrollment of people living with HIV in health care coverage.)
Broader Medicaid eligibility. Under the ACA, states have the option, which is fully Federally funded for the first three years, to expand Medicaid to generally include those with incomes at or below 138% of the Federal poverty line, including single adults without children who were previously not generally eligible for Medicaid. (Use this tool to find out if you qualify.) As of October 2023, 41 statesExit Disclaimer (including DC) have expanded Medicaid coverage. Medicaid is the largest payer for HIV care in the United States, and the expansion of Medicaid to low-income childless adults is particularly important for many gay, bisexual, and other men who have sex with men (MSM) who were previously ineligible for Medicaid, and yet remain the population most affected by the HIV epidemic. Further, in states that have opted for Medicaid expansion, people with HIV who meet the income threshold no longer have to wait for an AIDS diagnosis in order to become eligible for Medicaid. That means they can get into life-extending care and treatment before the disease has significantly damaged their immune system. (Find out if your state has expanded Medicaid coverage and if you qualify based on your household income.)
More affordable coverage. To help people access quality, affordable coverage, the ACA created the Healthcare.gov Marketplace (and some state-run Marketplaces, sometimes called “exchanges”) that help consumers compare different health plans and determine what savings they may qualify for. The ACA also provides financial assistance for people with low and middle incomes in the form of tax credits that lower the cost of their monthly premiums and lower their out-of-pocket costs. These tax credits depend on a family’s household size and income. In addition, Americans can apply for free or low-cost coverage through Medicaid and CHIP at any time, all year. If you qualify, coverage can begin immediately.
Lower prescription drug costs for Medicare recipients. In the past, as many as one in four seniors went without a prescription drug every year because they couldn’t afford it. The ACA closed, over time, the Medicare Part D prescription drug coverage gap once known as the donut hole—the gap between when a person’s initial Medicare drug coverage ended and when they qualified for catastrophic coverage. Previously, when people reached the donut hole, they had to pay the full cost for their prescription drugs until they reached the catastrophic coverage level and many struggled to pay for their medications. Under the ACA, the donut hole began shrinking in 2011 and closed in 2020. Now, people in the coverage gap will pay no more than 25% of the cost of their covered medications. Also, because of the ACA, AIDS Drug Assistance Program (ADAP) spending is now counted as part of Medicare Part D’s True Out-of-Pocket (“TrOOP”) costs, allowing ADAP clients who are Medicare Part D enrollees to reach the catastrophic coverage level faster, when Medicare starts covering the full cost of medications. (To learn more about your Medicare coverage and choices, visit Medicare.gov.)
Need Marketplace Health Coverage?
The Marketplace Open Enrollment Period for 2024 is closed. However, you can still get or change plans through a Special Enrollment Period if you have certain life events, like losing coverage, moving, getting married, or having a baby. Learn more about special enrollment opportunities.
Also, see if you qualify for Medicaid or CHIP. Medicaid and CHIP can provide free or low-cost health coverage to low-income people, families and children, pregnant women, the elderly, and people with disabilities. If you are eligible, you can enroll at any time; there is no open enrollment period. Find out if you qualify and get steps to apply.
Ensuring Quality Coverage
The Affordable Care Act also helps all Americans, including those with or at risk for HIV, have access to the best quality coverage and care. This includes:
Preventive services. Under the ACA, most new health insurance plans must cover certain recommended preventive services including HIV testing for everyone age 15 to 65 and other ages at increased risk without additional cost-sharing, such as copays or deductibles. Since about one in eight people with HIV in the U.S. (13%) are unaware of their HIV status, improving access to HIV testing will help more people learn their status so they can be connected to care and treatment. Pre-exposure prophylaxis (PrEP) to prevent HIV is also covered for HIV-negative adults at high risk for getting HIV through sex or injection drug use. This coverage of PrEP includes medications as well as necessary clinic visits and lab tests. Other preventive health services related to HIV risk and/or health outcomes are also covered, such as sexually transmitted infection counseling, syphilis screening, hepatitis B and hepatitis C screening, and hepatitis A and hepatitis B immunizations.
Comprehensive coverage. The law establishes a minimum set of benefits (called essential health benefits) that must be covered under health plans offered in the individual and small group markets, both inside and outside of the Health Insurance Marketplace. These include many health services that are important for people with HIV, including prescription drug services, hospital inpatient care, lab tests, services and devices to help you manage a chronic disease, and mental health and substance use disorder services, as well as HIV screening, PrEP, and other preventive services for those at risk for HIV.
Coordinated care for those with chronic health conditions. The law recognizes the value of patient-centered medical homes as an effective way to strengthen the quality of care, especially for people with complex chronic conditions such as HIV. The patient-centered medical home model of care can foster greater patient retention and higher quality HIV care because of its focus on treating the many needs of the patient at once and better coordination across medical specialties and support services. The Ryan White HIV/AIDS Program has been a pioneer in the development of this model in the HIV health care system. The ACA also authorized an optional Medicaid State Plan benefit for states to establish Health Homes to coordinate care for Medicaid beneficiaries with certain chronic health conditions. HIV/AIDS is one of the chronic health conditions that states may request approval to cover.
Enhancing the Capacity of the Healthcare Delivery System
The ACA expands the capacity of the healthcare delivery system to better serve all Americans, including those with and at risk for HIV. For example:
Expansion of community health centers. The ACA has made a major investment in expanding the network of community health centers that provide preventive and primary care services to nearly 30 million Americans every year, regardless of their ability to pay. Health centers provide high quality primary care services and support public health priorities such as the response to the opioid crisis, the implementation of the National HIV/AIDS Strategy and the Ending the HIV Epidemic in the U.S initiative (EHE), and the response to COVID-19. Learn more about HRSA-funded health centers, HIV, and viral hepatitis.
Delivering culturally competent care. The ACA expands initiatives to strengthen cultural competency training for all healthcare providers and ensure all populations are treated equitably. It also bolsters the Federal commitment to reducing health disparities. One effort underway to expand the capacity of health centers to deliver culturally competent care to populations heavily impacted by HIV is the National LGBTQIA+ Health Education CenterExit Disclaimer, funded by HRSA. This center helps healthcare organizations better address the needs of lesbian, gay, bisexual, transgender, queer, intersex, asexual, and all sexual and gender minority people, including individuals’ needs for HIV prevention, testing, and treatment.
Increasing the healthcare workforce for underserved communities. Thanks to the ACA, the National Health Service Corps is providing loan repayment and scholarships to more doctors, nurses, and other health care providers, a critical healthcare workforce expansion to better serve vulnerable populations. This is in line with a key recommendation of the National HIV/AIDS Strategy to increase the number and diversity of available providers of clinical care and related services for people with HIV, many of whom live in underserved communities.
Learn More About the Affordable Care Act
Here are several resources to help you stay informed about the Affordable Care Act and its impact on people with HIV:
- HealthCare.gov is the U.S. Department of Health and Human Services website to help you understand your health coverage options and compare health plans so you can enroll in a plan that works for you and your family.
- The Ryan White TARGETHIV Center's Health Coverage LibraryExit Disclaimer is a collection of resources to help Ryan White agencies and consumers better understand health care coverage.
- The Ryan White Access, Care, & Engagement (ACE) TA CenterExit Disclaimer helps Ryan White HIV/AIDS Program grantees and subgrantees enroll diverse clients, especially people of color, in health insurance and build provider cultural competence.
- NASTADExit Disclaimer (formerly the National Alliance for State and Territorial AIDS Directors) offers resources about health reform efforts and how they may affect people living with HIV/AIDS.
- Greater Than AIDS: Health Coverage, HIV and YouExit Disclaimer is a site developed by the Kaiser Family Foundation to help people living with HIV learn about their coverage options and how the law could affect their care and treatment.